No Sirens, No Flashing Lights: ‘Mental Health Ambulances’ Available For Utahns In Distress
Sep 12, 2019, 7:38 PM | Updated: Sep 13, 2019, 9:53 am
SALT LAKE CITY, Utah – Knowing what to do in the middle of an immediate mental health crisis can be overwhelming. Many people immediately call 9-1-1, but that might not always be the best option. An underutilized service without flashing lights and sirens offers a less threatening approach for Utahns.
Rep. Steve Eliason, R-Sandy, said he focuses much of his legislative work on suicide prevention. “I know somebody who was experiencing a mental health crisis and they called emergency services for help,” he said.
The woman called 9-1-1 and “they sent out a fire truck, ambulance and police car,” Eliason said. “The response to the neighborhood of all of these vehicles with flashing lights, for her, created more of a crisis than what she was actually calling first to seek help for.”

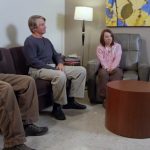
MCOT members show up in pairs made up of a licensed clinical social worker and a certified peer support specialist.
Eliason said there is a better, underutilized option available. It’s called MCOT — the Mobile Crisis Outreach Team. “It’s kind of like a mental health ambulance with a clinician and somebody who has experienced maybe something similar to what this person’s experiencing so they can relate with them,” he said.
But unlike traditional emergency service vehicles with EMS branding, flashing lights and sirens, MCOT units are unmarked vehicles and are designed to look like any other car on the road. They’re discreet and don’t draw unnecessary attention.
“The whole lights, sirens, that’s not necessary,” said Gina, who’s a certified social worker at the University Neuropsychiatric Institute. “Police can at times be intimidating, and sometimes it can lead to other unnecessary barriers to actually getting their mental health stuff figured out.”
When someone in Utah calls the National Suicide Hotline in distress, they’re connected to the University Neuropsychiatric Institute call center in Salt Lake.
“Sometimes we feel unsafe with ourselves, sometimes we don’t know what to do,” Gina said. “Sometimes our families don’t feel safe to be around us. We problem-solve with them. We make that quick, in person, ‘Hey, how are you? Today’s a bad day? Tell me about it.'”
If needed, a licensed clinical social worker and certified peer support specialist go in pairs directly to the patient in street clothes, rather than uniforms.
“We’re humans who know a lot about mental health,” Gina said. “We can support you through this because sometimes family can’t really support you. It’s too heavy. It’s too hard, but I think one thing that I found is, it’s important to know that you’re not alone. You don’t have to do this alone. You don’t have to walk this path alone. There’s someone out there.”
For most — it’s enough. “The vast majority of the individuals that receive services may have caught are able to be stabilized in their home avoiding a trip to the hospital,” Eliason said.
It also helps the patient avoid steep and unnecessary bills. “I mean, the average ambulance ride could be over $1,000,” Eliason said.
MCOT service is free and available 24/7, but if the patient needs further attention, officials will coordinate a trip to the hospital, day treatment services or other therapy.
“They’ll also follow up with them in the day subsequent to this person’s crisis, to see how they’re doing, and see if they’re in need of additional services,” Eliason said. “They work on short term coping strategies and long term recovery ideas, which the ultimate goal is to get people back on their feet, being happy again.”
If necessary, MCOT will work hand in hand with traditional EMS and law enforcement to protect someone in immediate harm or danger or others around them.
Unlike traditional emergency services, most peer support specialists have been on the other side of the service, like Kevin, who said his own experience helps him relate to his patients.
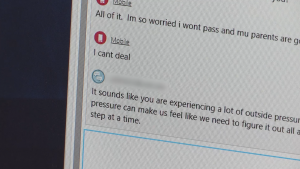
People in distress can call the National Suicide Hotline or chat with a licensed social worker online.
“I have the scars,” he said. “People pay attention to that because they know you lived through it, and you have a story to tell. Who better to handle that situation than somebody who’s been in it before? Or at least been through something like it?”
His experience gives his words of encouragement and hope extra meaning. “That’s one of the most important things is that as black as it gets, there’s still hope,” he said.
MCOT units currently dispatch in Salt Lake, Davis, Weber and Utah counties and the southwest region of Utah, including St. George and surrounding cities.
Eliason said he has plans to expand the program to more rural areas and to start tele-health MCOT services in the next legislative session.
“It’s important to know that MCOT’s are not just not a new idea that we’re trying in Utah,” he said. “This is a national best practice and states that have really developed their mental health crisis response system heavily use MCOT’s. It’s the wave of the future.”
The first MCOT started in Salt Lake in 2012 and at it’s busiest can send up to six teams throughout Salt Lake County.
Eliason said he hopes more people learn and use this free service.
____________________________
Suicide Prevention Resources
If you or someone you know is experiencing suicidal thoughts or exhibiting warning signs, call the Utah Statewide CrisisLine in affiliation with the National Suicide Prevention Lifeline: 1-800-273-TALK (8255).
Or, you can directly call the Utah Statewide CrisisLine: 801-587-3000
Additional Crisis Hotlines
- Utah County Crisis Line: 801-226-4433
- Salt Lake County/UNI Crisis Line: 801-587-3000
- Wasatch Mental Health Crisis Line: 801-373-7393
- National Suicide Prevention Crisis Text Line: Text “HOME” to 741-741
- Trevor Project Hotline for LGBTQ teens: 1-866-488-7386
- University Of Utah Crisis Interventional Crisis Line: 801-587-300
Online Resources
- NAMI Utah
- Utah Chapter-American Foundation for Suicide Prevention
- Suicide Prevention Lifeline
- Safe UT Crisis Text and Tip Line
In an emergency
- Call the police
- Go to the emergency room