Former KSL anchor avoids life-changing surgery by learning genetic risk
Mar 14, 2023, 9:35 AM
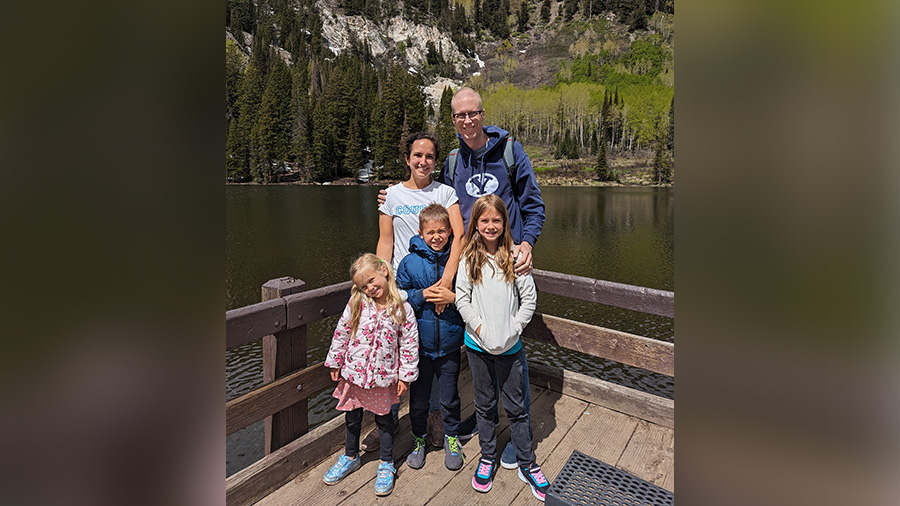
SALT LAKE CITY — For the last seven months, former KSL news anchor Keith McCord has felt like a human pin cushion. Each week, he needed to get rid of a bag of blood.
“This was Monday’s stick, so let’s do this one,” he said as he gave his arm to the phlebotomy nurse.
It was treatment for a genetic condition he didn’t know he had, identified in a study about which he’d forgotten. He got a letter from Intermountain Health.
“It said you may have tested positive for a mutated gene and it could affect your long-term health,” McCord said.
McCord had hemochromatosis, which means his body accumulates iron. A normal person would measure under 100 nanograms per milliliter of iron. McCord’s iron levels were close to 2,000.
“The iron level was off the chart, so that alarmed them. They said we need to do something,” he said.
If you could learn your risk for serious health problems in the future would you? My friend and colleague @KeithMcCord prevented life changing surgery by taking part in @Intermountain HerediGene. Watch on @KSL5TV at 10. pic.twitter.com/tn4Mf9rzP9
— Deanie Wimmer (@DeanieWimmer) March 12, 2023
He had no symptoms and no clue. Thankfully, he’d signed up for Intermountain Health’s HerediGene study five years ago after heart surgery, and they caught it.
“In Keith’s case, it would have presented as a need for a liver transplant or something very significant. Instead, we caught it early and it could be dealt with in a much more reasonable way,” said Dr. Howard Mcleod, executive clinical director of Precision Health, Intermountain Health.
Those months of admittedly annoying blood draws prevented a life-changing surgery. That is one potential impact of HerediGene.
HerediGene is the country’s largest DNA study, conducted by Utah’s Intermountain Health. Through blood draws, it maps the genome of participants to determine their risk of everything from cancer to heart disease to diabetes.
“You don’t know what is sitting there, and in some cases, you can know what’s sitting there and do something about it before it becomes a problem,” Mcleod said.
And they’ve been doing that with a frequency that surprised even them. In the first group of 25,000 participants, nearly 4,000 had health risks so urgent, researchers dropped what they’re doing and contacted the patient.
“So that was much higher than anticipated,” Mcleod said.
Intermountain Health gathers valuable research as they see new trends and even new health risks emerge. By identifying problems early, HerediGene also has the potential to revolutionize the cost of health care.
It is difficult to get and compare health costs. Intermountain told us they couldn’t provide them.
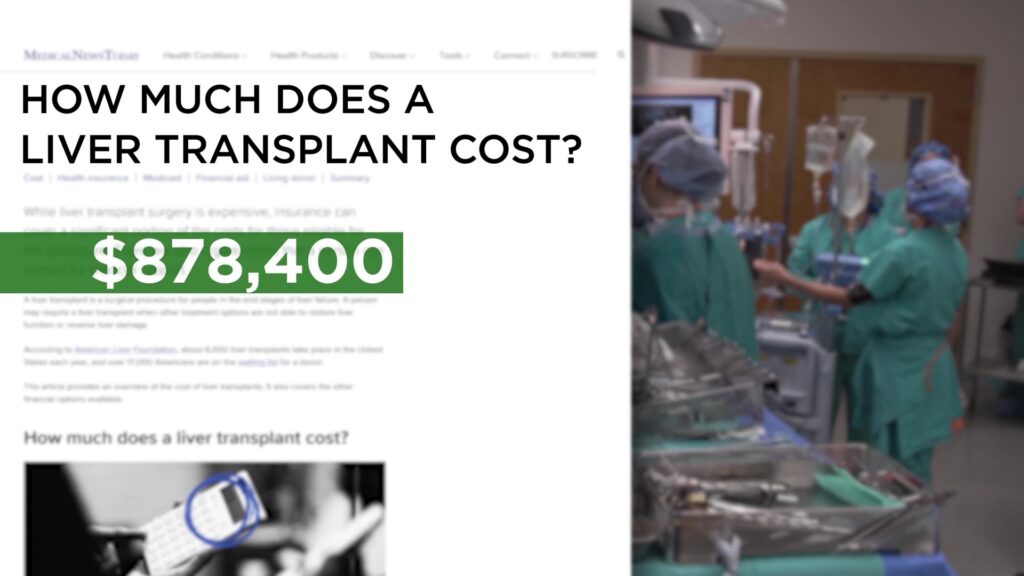
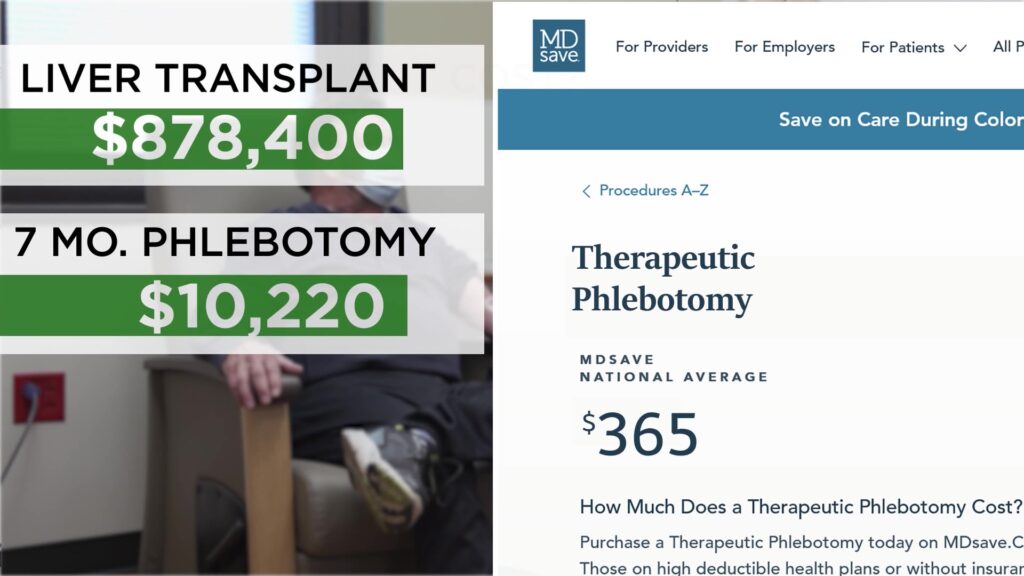
According to Medical News Today, in 2020, the costs associated with a liver transplant before insurance can run as high as $878,000.
The website MDSave shows the average cost of McCord’s therapeutic phlebotomy is $365. Once a week for seven months, the total cost — $10,220.
“This could be a big breakthrough in the future of medicine and treatment, that kind of stuff,” McCord said. “If you can avoid getting a bad disease, that’s a big deal.”
HerediGene is enrolling about 7,000 patients each month. Many, like McCord, find insurance will cover the cost of their treatments.
“By identifying genetic risk, we can get a little bit of a glimpse into the crystal ball of that person’s health,” Mcleod said.
For more information, click here.