Get Gephardt: Exception in federal law leaves patients still facing surprise medical bills for ambulance rides
May 4, 2023, 6:31 AM | Updated: 6:45 am
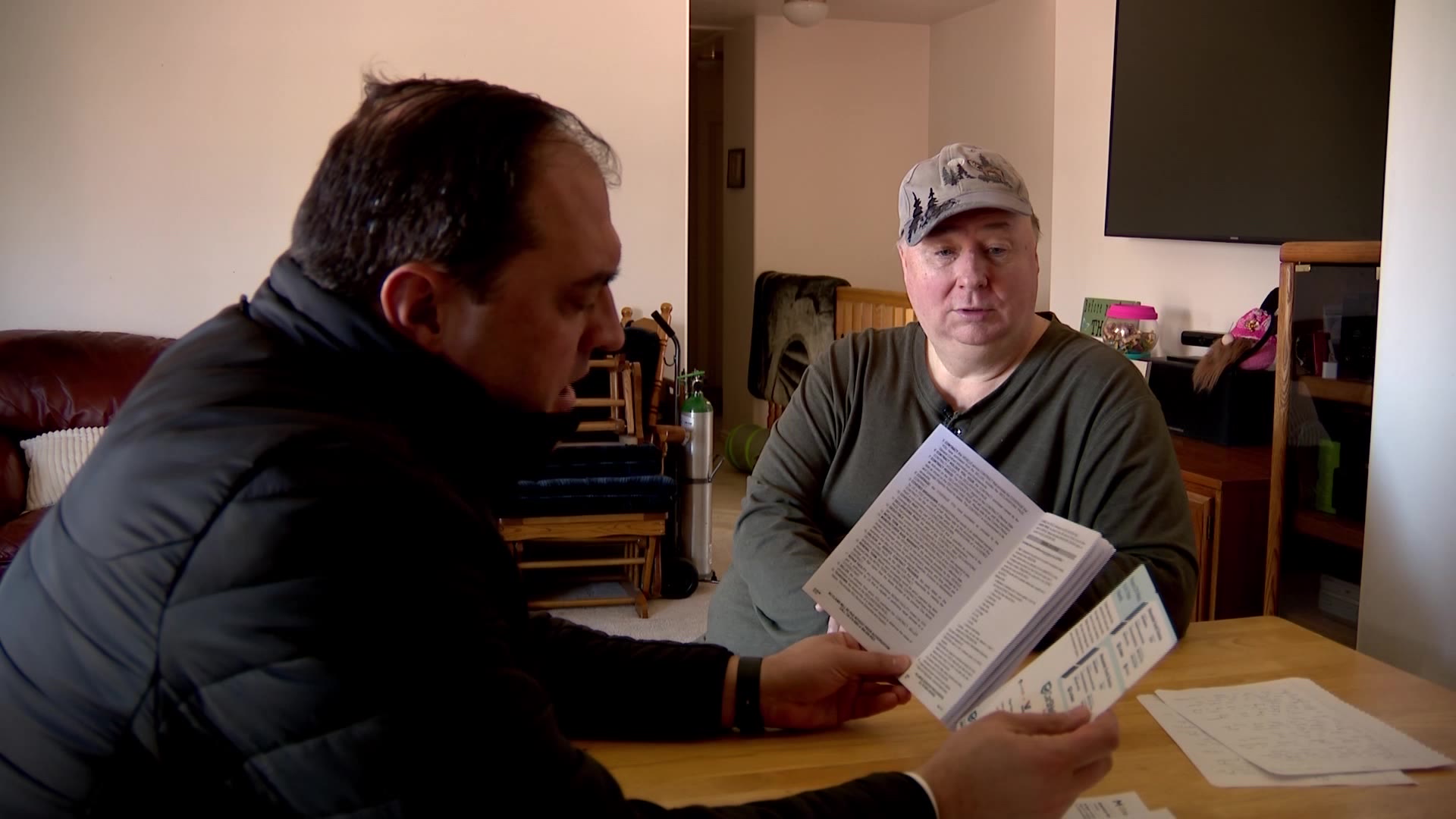
TAYLORSVILLE, Utah — More than a year ago, Chris Wilcox rushed his 6-month-old to the nearest hospital where doctors told him it was RSV, and it was urgent.
“They said that we needed to send him to Primary Children’s Hospital,” Wilcox said.
It wasn’t a long trip, about a half-hour drive going the speed limit. Wilcox said he asked the doctor if he could drive his son himself in his car.
“The doctor said that he did not recommend that and if it was his child that he would use the ambulance,” Wilcox said.
Wilcox followed the doctor’s orders and, after a brief stint in the ER, the kid was sent home.
More than a year later, Wilcox got a surprise bill from the ambulance company.
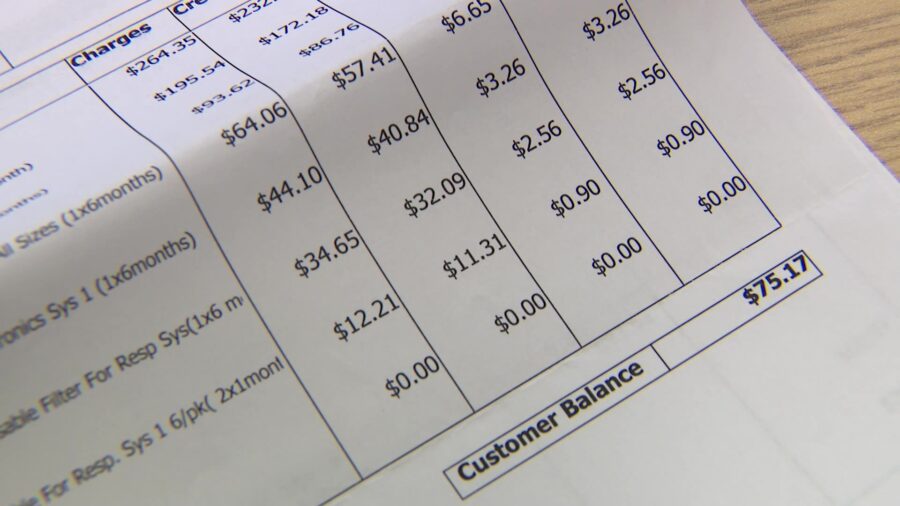
“We could be forced to pay $2,500 plus mileage for the ambulance trip,” he said.
Wilcox said he pressed both the ambulance company, Gold Cross, and his insurance company, Molina, for an explanation for what seemed like a pretty high bill. He learned that even though both hospitals were in-network, the ambulance was “out-of-network.”
“It’s difficult when insurance doesn’t cover the things that it’s intended to cover,” Wilcox said.
In 2022, Congress passed the “No Surprises Act,” which was supposed to end surprise medical bills when someone, in a medical emergency, ends up dealing with an “out of network” provider. But look a little closer, and you’ll see an important exception; the act does not apply to “ground ambulance services.”
Gold Cross President Mike Moffit said in Utah, ambulance rates are set by state law, and that is the rate they charged for transporting Wilcox’s child. Moffitt said they’ve been trying to convince Molina to pay more ever since. Moffit said dealing with Molina has been frustrating.
“It’s a runaround. Send us this. Send us that. Send us another piece of paper and we’ll ignore you for another three months,” Moffit said.
Moffit says they went round and round and Molina “finally paid us less than half of what the billed amount was.”
It left Moffit with a bill of more than $1,500.
“It ends up still being the patient’s responsibility,” Moffit said.
KSL TV reached out to Molina, asking questions like how come they “paid less than 50% of the cost” and “Why aren’t these costs paid at a higher level since Utah has set caps on how much ambulance companies can charge for services?”
Molina’s spokesperson didn’t answer those questions, simply writing in an email, “The issue has been resolved directly with the member.”
Emails from KSL TV attempting to follow up with Molina were unanswered.
As for Wilcox, he tells us Molina finally paid the rest, leaving him to pay his $130 copay.
He’s happy about his resolution but said he thinks people need to know that the law carves out a special exception for ambulances — and it can be costly for patients.
“We think that emergency service will be covered. However, for some reason, this is exempted from that,” he said.
The federal government does have a mediator, of sorts, to whom patients can turn when there are payment disputes between providers and health plans. But it won’t help with ambulance bills, which are state regulated.